Module 1: The Cardiovascular System
Introduction
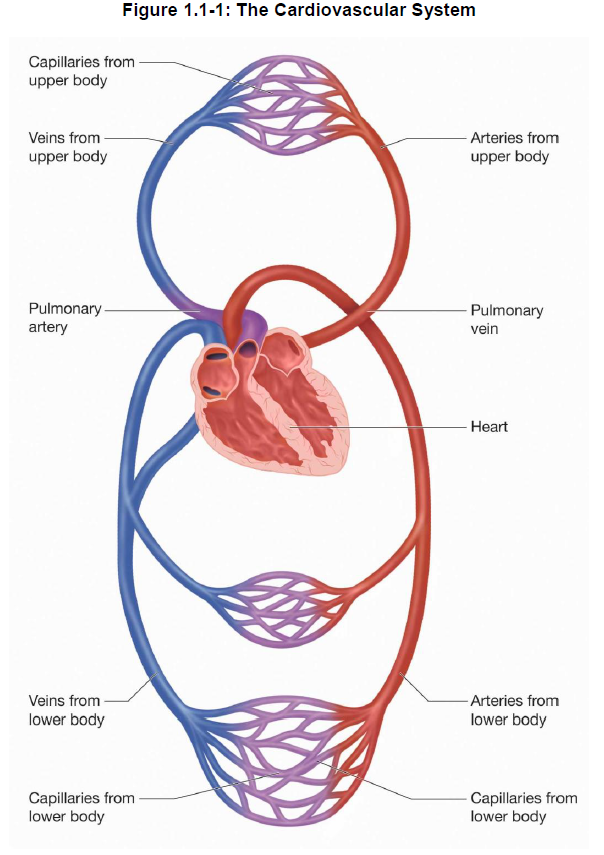
The cardiovascular system is a closed system composed of the heart, blood vessels and blood. The pumping action of the heart forces the blood through the many blood vessels. The heart is only slightly bigger than a clenched fist. Through its pumping action, it ensures that blood is circulated through the body to meet the body’s metabolic needs. Blood transports nutrients, oxygen, and other substances to body cells and helps rid the body of waste materials. Lymphatic vessels work in conjunction with the cardiovascular system.
In this module, we discuss the anatomy and physiology of the components of the cardiovascular system.
Module Structure
This module is divided into 4 sections:
Section 1: Overview of the Cardiovascular System
Section 2: Anatomy and Physiology of Blood Vessels
Section 3: Anatomy and Physiology of the Heart
Section 4: Function and Composition of Blood
Learning Objectives
After reading this section, you should be able to:
- State the function of the cardiovascular system.
- List the major components of the cardiovascular system and state the function of each.
- Differentiate between pulmonary and systemic circulation.
- State the function of the lymphatic system.
Function of the Cardiovascular System
The cardiovascular system transports nutrients, oxygen and other substances in the blood to all body cells and carries wastes away from the cells. The needs of the tissues and cells vary according to their changing levels of activity. The cardiovascular system is designed to accommodate the varying needs of all body tissues by delivering the amount of blood to the tissue that is necessary for its function and survival.
Components of the Cardiovascular System
The cardiovascular system has three major components:
-
-
- blood vessels
- heart
- blood
-
The heart is a pump that can vary its output. The pumping action of the heart forces the blood through the hollow blood vessels.
Blood carries life sustaining oxygen, nutrients, hormones, electrolytes and heat to every living cell. Simultaneously, the blood collects wastes such as carbon dioxide, urea*, and extra water and heat from the cells. Heat is carried in blood to the skin where it is dissipated. Blood flow to the skin is increased when body temperature rises and is decreased when body temperature falls. During exercise, body temperature rises. Thus, the blood flow to the skin increases in order to release this increased heat through sweat.
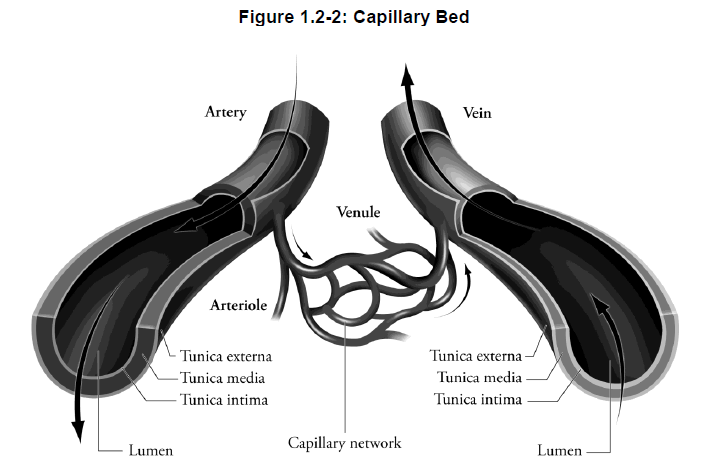
Structure of the Cardiovascular System
The cardiovascular system is a closed, one-way system (see Figure 1.1-1). Blood is continuously pumped out of the heart through one set of blood vessels, the arteries*, and returned to the heart via another, the veins*. In between the arteries and veins are arterioles, capillaries* and venules. Arterioles are small arteries that deliver blood to the capillaries. Capillaries are very small vessels that allow single red blood cells to pass through. Capillaries release oxygen and deliver nutrients to the body cells and at the same time, they pick up waste from the cells. When small capillaries unite, they form small veins called venules. Venules collect blood from the capillaries and drain it into veins.
Blood flows within two principal circulating systems, the pulmonary circulation and systemic circulation.
-
-
- pulmonary circulation – blood flows from the right side of the heart to the lungs, and back to the left side of the heart
- systemic circulation system – transports blood from the left side of the heart through the blood vessels serving the remainder of the body (except the lungs), and back to the right side of the heart
-
The systemic system can be thought of as a delivery system for oxygen and nutrients, while the pulmonary system can be viewed as an oxygen reservoir from the lungs. These two systems work in a coordinated manner to meet the body’s oxygen and energy needs. They meet in the heart, with the right side of the heart pumping the pulmonary circulation, and the left side of the heart completing the systemic circulation.
Lymphatic System
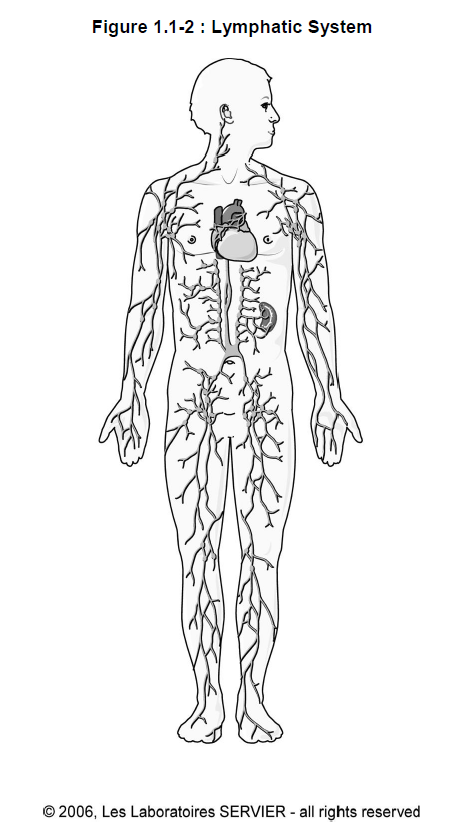
Water and dissolved substances constantly move through the capillary walls into the spaces between cells and add to the volume of tissue fluid. Under normal conditions, this fluid is constantly removed so that it does not accumulate in the tissues.
Some of the fluid moves back into the capillaries by diffusion. The lymphatic system is another pathway for the fluid to re-enter the circulatory system. The lymphatic system also carries proteins and large particulate matter away from tissues and returns them to the blood stream. This is an essential function.
Like the cardiovascular system, the lymphatic system also contains vessels and capillaries. The lymphatic capillaries drain away excess tissue fluid, proteins and other matter that does not return to the blood capillaries. Eventually this fluid, called lymph*, is emptied into the circulatory system.
Lymph from the lower body flows up the thoracic duct and empties into the venous system at the juncture of the left internal jugular vein and subclavian vein. Lymph from the upper body enters at the same juncture on either the right of left side of the body.
Summary — Section 1: Overview of the Cardiovascular System
The cardiovascular system is a closed, one-way system that delivers nutrients, oxygen and other substances to body cells, and collects wastes from cells of the body.
Blood vessels, the heart, and blood make up the cardiovascular system.
Blood flow is described in terms of pulmonary circulation and systemic circulation. Blood flow within the pulmonary circulation originates from the right side of the heart, flows through the lungs and back to the left side of the heart. The systemic circulation circulates blood from the left side of the heart through body tissue and back to the right side of the heart.
The lymphatic system contains vessels and capillaries that drain excess tissue fluid and eventually empty the fluid, known as lymph, into the circulatory system.
Progress Check — Section 1: Overview of the Cardiovascular System
1.
Why is the body dependent on the cardiovascular system?
____________________________
____________________________
____________________________
2.
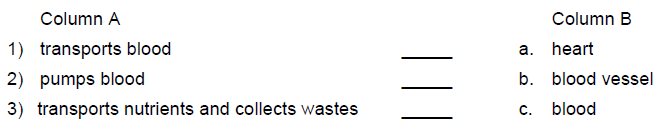
Match the function of the circulatory system in Column A with the correct cardiovascular system component in Column B.
3.
Differentiate between pulmonary and systemic circulation.
____________________________
____________________________
____________________________
4.
What is the function of the lymphatic system?
____________________________
____________________________
____________________________
Progress Check Answers — Section 1: Overview of the Cardiovascular System
1.
The body relies on the cardiovascular system to deliver nutrients, oxygen, hormones, electrolytes and heat to all parts of the body and to collect wastes such as carbon dioxide, urea, and extra water and heat from the cells.
2.
1) blood vessel
2) heart
3) blood
3.
Pulmonary circulation is the flow of blood from the right side of the heart to the lungs to be oxygenated and back to the left side of the heart.
Systemic circulation is the flow of blood from the left side of the heart to all parts of the body via the arterial system, except the lungs, and back to the right side of the heart via the venous system.
4.
The lymphatic system collects excess tissue fluid (lymph) and returns it to the circulatory system.
Section 2: Anatomy and Physiology of Blood Vessels
Learning Objectives
After reading this section, you should be able to:
- Compare the structure and function of the arteries, veins and capillaries.
- Compare the components and function of the pulmonary, systemic and cardiac circulatory systems.
- Explain how the oxygen content of blood is maintained.
- Explain how the volume of blood flow is regulated.
- Define blood pressure.
- Explain the effect of cardiac output and peripheral vascular resistance on blood pressure.
- Describe the role of the sympathetic nerves, parasympathetic nerves, hormones, and the kidneys in the regulation of blood flow in the blood vessels.
- Describe the role of baroreceptors and the cardiovascular centre in the regulation of blood pressure.
Function of Blood Vessels
There are three basic types of blood vessels:
-
-
- arteries
- veins
- capillaries
-
Each type of vessel has a unique function.
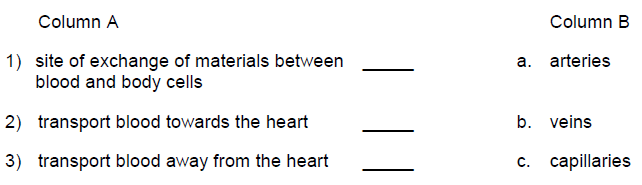
1) Arteries
Arteries carry blood away from the heart. Typically, this is oxygen rich blood. The pulmonary arteries* are an exception as they carry deoxygenated (oxygen poor) blood from the heart to the lungs. Arteries branch into smaller vessels called arterioles.
2) Veins
Veins carry deoxygenated blood back to the heart. The pulmonary veins* are an exception as they carry oxygenated (oxygen rich) blood back to the heart from the lungs. The smallest veins are called venules.
3) Capillaries
Capillaries connect the arterioles and venules. They are the sites of exchange of materials between the blood and body cells, or between the blood and the air in the lungs.
Structure of Blood Vessels
1) Arteries and arterioles
Arteries vary in size from about 25-35 mm in diameter (the aorta*), to about 0.5 mm in diameter.
Artery walls have three layers:
-
-
- thin innermost layer (intima) – consists of endothelium and some connective tissue
- thick intermediate layer (media) – composed of smooth muscle and connective tissue with elastic properties
- outer layer (adventitia) – consists of fibrous connective tissue and at times, smooth muscle
-
Their elastic properties allow large arteries to stretch during the pumping cycle of the heart. Without this elasticity the flow of blood would be intermittent rather than continuous through the circulatory system. (See Figure 1.2-1.)
The arterioles are arbitrarily defined as arteries that are under 0.05 mm in diameter. Arterioles, in comparison to arteries, contain a greater amount of smooth muscle than elastic tissue in the middle layer. Arterioles play a major role in regulating blood pressure*. By varying their internal size, they can vary their resistance. Varying resistance allows the redistribution of blood to organs in specific circumstances. For example, during exercise, blood is mostly redistributed towards the muscles and the blood is restricted from the GI tract.
Did You Know?
The aorta is the largest artery.
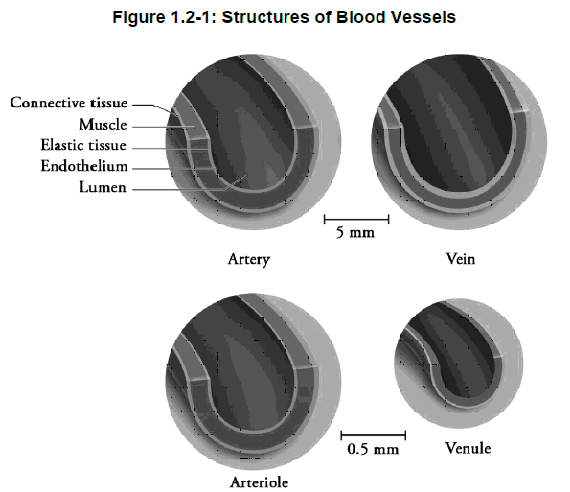
2) Veins and venules
The lumen* of veins is slightly larger in diameter than arteries, but veins are thinner walled than arteries. Vein walls have the same structure consisting of endothelial tissue, elastic tissue, muscle and connective tissue. However, they have only minimal amounts of elastic and smooth muscle tissue. (See Figure 1.2‑1.)
To move blood, the veins depend mainly on the contraction of skeletal muscle around them. Valves are found within veins, especially in the veins of the lower extremities. The valves ensure that blood flows towards the heart, even against the force of gravity. Blood is allowed to flow freely toward the heart but when blood reverses its direction of flow, the valves close and prevent the backflow of blood.
Venules, which are post-capillary vessels, have a lumen diameter similar in size to the arterioles. Their walls, however, have only an endothelial lining and a small amount of fibrous connective tissue in comparison to the thick walls of the arterioles.
3) Capillaries
Capillary vessels are very small, about 0.008 mm in diameter. Usually this is just wide enough to allow passage of a single red blood cell. In addition, each capillary is short in length (about 1 mm or less), but together they have a length in the thousands of miles and a surface area of nearly 6,000 square meters. The capillary wall consists only of endothelial cells, forming a layer one cell thick. This allows easy diffusion of nutrients and waste products across the capillary.
The capillaries and their associated structures (terminal arterioles and post-capillary venules) make up the microcirculation (see Figure 1.2-2). The primary function of the microcirculation is the exchange of nutrients and metabolic waste products. All other components of the circulatory system serve to deliver an adequate blood flow to the capillaries. The capillaries penetrate almost every tissue in the body.
Circulation Systems
As we discussed earlier, the two main circulatory systems in the body are the systemic circulation system and the pulmonary circulation system. The heart itself is supplied with blood by the cardiac circulation system (coronary circulation).
1) Pulmonary circulation
In the pulmonary circulation, blood flows from the right half of the heart through the lungs and returns to the left half of the heart.
Deoxygenated blood returning to the heart from the body leaves the right half of the heart via one large artery, the pulmonary artery. The pulmonary artery divides into two arteries, one supplying each lung. The pulmonary arteries are the only arteries that carry deoxygenated blood.
Within the lungs, the arteries branch into arterioles and ultimately capillaries. The capillaries unite to form venules, which in turn unite to form veins and finally large pulmonary veins, which drain into the left half of the heart. The pulmonary veins are the only veins that carry oxygenated blood.
2) Systemic circulation
The systemic circulation circulates blood from the left half of the heart to all the tissues of the body (except the lungs), and returns to the right half of the heart.
In the systemic circulation, blood leaves the left side of the heart via one large artery, the aorta. The aorta then branches into arteries that distribute blood under high pressure to the various organs and tissues of the body. Blood flows from regions of higher pressure to regions of lower pressure.
Two large veins, the inferior vena cava (from the lower portion of the body) and the superior vena cava (from the upper portion of the body) transport blood back to the right side of the heart.
Did You Know?
Pulmonary arteries are the only arteries that carry deoxygenated blood and pulmonary veins are the only veins that carry oxygenated blood.The system of blood vessels – arteries, veins and capillaries – is over 60,000 miles long. Blood takes about 20 seconds to circulate throughout the entire vascular system.
3) Coronary circulation
The first branches of the aorta are the right and left coronary arteries. These arteries supply the heart muscle with blood.
Blood within the systemic veins, pulmonary arteries and the right half of the heart has low oxygen content.
As the blood flows through the lung capillaries, the erythrocytes (also called red blood cells) absorb inhaled oxygen, increasing the oxygen content.
With passage of blood through the systemic capillaries, oxygen is utilized by cells and results in the low oxygen content of systemic venous blood.
Blood Flow
The cardiovascular system meets the demands of the body for oxygen and nutrients by adjusting the flow of blood to parts of the body. The volume of blood is regulated by changing the size of the blood vessels.
Vasodilation* is an increase in the diameter of a vessel and results in increased blood flow. Vasoconstriction* is a decrease in the diameter of a blood vessel, resulting in a decrease in blood flow.
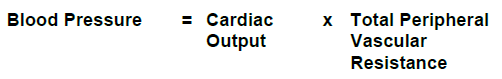
Blood Pressure
Blood pressure is the force exerted by the blood against the walls of the vessels.
Blood pressure varies with the amount of blood being pumped by the heart (cardiac output*) and the resistance presented by the blood vessels (total peripheral vascular resistance*).
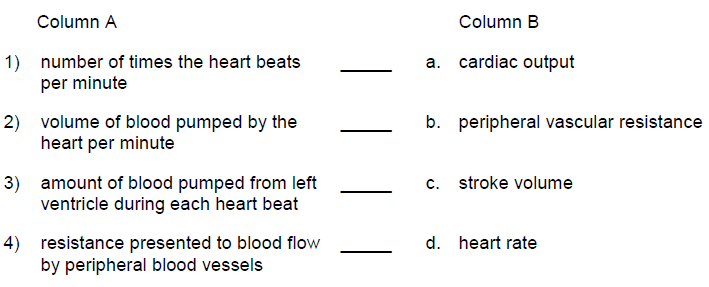
Cardiac Output
Cardiac output (CO) is the volume of blood pumped out each minute from the left ventricle* of the heart. Cardiac output is affected by heart rate* and stroke volume*.
1) Heart rate (HR)
The heart can vary its output by increasing the number of times it beats per minute (referred to as the heart rate). When a person exercises, the HR increases, resulting in an increase in the cardiac output.
2) Stroke volume (SV)
With each contraction, the heart pumps out a certain amount of blood. The heart can vary this output by changing the stroke volume.
Peripheral Vascular Resistance
Peripheral vascular resistance (PVR) refers to the amount of resistance that blood encounters as it flows through the blood vessels. Resistance to blood flow in blood vessels is affected by the blood vessel length, by the blood vessel radius and by the viscosity of the blood.
The peripheral vascular resistance is defined through this equation:
1) Blood vessel length
As illustrated in the equation above, the length of the vessel is proportional to the peripheral vascular resistance. The longer the length of the vessel, the greater the resistance will be. For example, an obese patient will have an increased total vessel length as it needs more vessels to feed all the cells.
2) Radius of a vessel (size of a vessel)
As illustrated in the equation above, the radius of the vessel is inversely proportional to the peripheral vascular resistance. The change in this variable leads to the biggest changes in resistance. The smaller the radius of the vessel, the greater the resistance will be.
3) Blood viscosity
The thickness (viscosity) of blood will determine its ability to flow. Normally, the viscosity of blood does not change, and therefore, plays a minor role.
Did You Know?
Increased peripheral vascular resistance is the main cause of elevated blood pressure (hypertension).
Importance of Maintenance of Blood Pressure
To ensure that adequate amounts of blood reach all body tissues, blood pressure must be regulated and maintained within normal limits.
Blood pressure raised above normal values, also called (hypertension*, can cause damage to the vascular system and other organs.
If the brain and/or other vital organs of the body do not receive adequate amounts of blood (ischemia*) for an extended period of time due to a drop in blood pressure, then their cells may die and organ death could result.
Regulation of Blood Pressure
Hormones, the renal system, and the nervous system regulate blood pressure.
1) Hormonal control of blood pressure
The adrenal gland controls the release of the hormones epinephrine* and norepinephrine*, and the nervous system releases norepinephrine in response to changes in blood pressure. These hormones are vasoconstrictors.
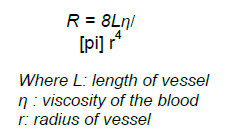
2) Renal control of blood pressure
The renin-angiotensin-aldosterone (RAA) system* provides a means to maintain control of cardiac hemodynamics.
If blood pressure drops in the kidneys, specialized cells in the kidneys produce the enzyme renin*, which promotes the conversion of angiotensinogen to angiotensin I*. Angiotensin I is converted to angiotensin II* by the action of angiotensin converting enzyme (ACE)*. Angiotensin II acts as a vasoconstrictor and also increases the production of another hormone, aldosterone*, which leads to an increase in sodium and water reabsorption by the kidney which increases the blood volume. These two effects act in concert to raise blood pressure. The renin-angiotensin-aldosterone system is explained in greater detail in Module 2: The Urinary System.
3) Nervous system control
A cardiovascular control centre is located in the medulla of the brain. The medulla receives messages from specialized nerve cells (baroreceptors*) located in the walls of the aorta, carotid arteries, heart, and pulmonary vessels. Changes in vascular resistance occur to compensate for changes in arterial blood pressure.
Messages from another part of the brain called the hypothalamus* also are received by the medulla and are used to help regulate the flow of blood.
Messages from the medulla are transported by both the sympathetic and parasympathetic nervous system. Neurons* from both nervous systems directly innervate various tissues in the heart. All blood vessels, except capillaries and venules, which do not contain smooth muscle, are innervated by the sympathetic nervous system. The parasympathetic nerves have little or no effect on the blood vessels.
Baroreceptor Reflexes
The baroreceptor reflex is the body’s rapid response system for dealing with changes in blood pressure. Baroreceptors are stretch receptors that convey messages to the cardioacceleratory centre and the cardioinhibitory centre of the medulla. They are found in the aortic arch, in the walls of the carotid arteries, right and left atria* and left ventricle of the heart, and in pulmonary vessels.
1) Decrease in blood pressure
A decrease in blood pressure results in a decreased rate of firing of the baroreceptors. This stimulates the cardioacceleratory centre. This increases sympathetic outflow and inhibits the cardioinhibitory centre, which decreases parasympathetic outflow.
The adrenal medulla is also stimulated to release epinephrine and norepinephrine. The blood pressure will increase due to vasoconstriction, increased heart rate, increased force of contraction, and increased cardiac output.
2) Increase in blood pressure
With increased blood pressure, baroreceptor firing increases resulting in the stimulation of the cardioinhibitory centre and inhibition of the cardioacceleratory centre.
The net result is a decreased heart rate, decreased strength of contraction and vasodilation.
Sympathetic Nervous System
Sympathetic nerve fibres originate in the cardioacceleratory centre of the medulla. They are usually adrenergic* and thus release adrenaline (epinephrine) and noradrenaline (norepinephrine).
Stimulation of the sympathetic nervous system causes muscle fibres in the blood vessel walls to either dilate or constrict. In the heart, stimulation of the sympathetic nerves increases the heart rate and the strength of the contraction of the heart. This results in increased cardiac output.
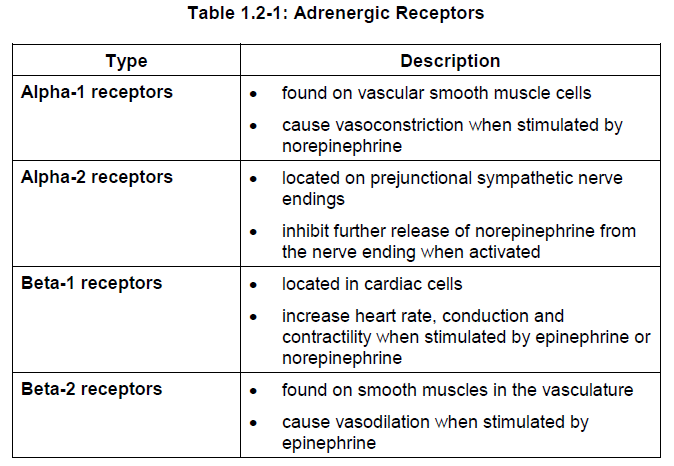
Various tissues have differences in the type and number of adrenergic receptors. Adrenergic receptors consist of alpha and beta‑receptors. These receptors can be further subdivided into alpha-1 and alpha-2, as well as beta-1 and beta-2 subtypes.
Parasympathetic Nervous System
Parasympathetic neurons originate in the cardioinhibitory centre in the medulla of the brain.
Stimulation of these neurons results in a release of acetylcholine (ACh) *, which decreases the heart rate.
In addition, conduction of the electrical impulse through the heart and the strength of cardiac contraction are decreased (negative inotropic* response).
The parasympathetic nerves have little or no effect on the blood vessels.
Summary — Section 2: Anatomy and Physiology of Blood Vessels
The three basic types of blood vessels are the arteries, veins, and capillaries. These blood vessels vary in diameter, thickness of the vessel wall, and the relative amounts of endothelial tissue, elastic tissue, smooth muscle tissue, and connective tissue. Arteries are able to stretch during the pumping cycle of the heart to allow for a continuous flow of blood. Veins contain valves, which aid in the flow of blood back to the heart. Capillary walls consist of only one layer of endothelial cells. Therefore, nutrients and wastes are able to diffuse across the capillary walls.
Vasodilation and vasoconstriction of the vessels regulate the volume of blood being transported to different parts of the body.
Blood pressure is the force exerted by the blood against the wall of the blood vessels. Blood pressure is determined by cardiac output (CO) and peripheral vascular resistance (PVR). Cardiac output is in turn determined by heart rate (HR) and stroke volume (SV). Peripheral resistance is affected by blood vessel size, blood vessel elasticity, and blood viscosity.
Blood pressure is also regulated by the hormones epinephrine and norepinephrine, the renin-angiotensin-aldosterone system, serum sodium and the cardiovascular centre located in the medulla of the brain. The cardiovascular centre receives messages from baroreceptors, which are located in the aorta, carotid arteries, atria and ventricles of the heart, and pulmonary vessels, as well as from the hypothalamus.
Stimulation of the sympathetic neurons causes muscle fibres in the blood vessel walls to either dilate or constrict. In the heart, stimulation of the sympathetic nerves increases the heart rate and the strength of the contraction of the heart, resulting in increased cardiac output. Sympathetic nerves are usually adrenergic and release norepinephrine (noradrenaline) and epinephrine (adrenaline). Alpha-1 adrenergic receptors located in vascular smooth muscle cells cause vasoconstriction when stimulated by norepinephrine. Alpha-2 receptors located on prejunctional sympathetic nerve endings inhibit further release of norepinephrine when activated. Beta-1 receptors located in cardiac cells cause increased heart rate, conduction and contractility when stimulated by epinephrine. Beta-2 receptors located on smooth vascular muscles cause vasodilation when stimulated by epinephrine.
Parasympathetic neurons release acetylcholine, which decreases the heart rate, conduction through the heart and the strength of cardiac contraction. Parasympathetic neurons have little or no effect on the blood vessels.
Progress Check — Section 2: Anatomy and Physiology of Blood Vessels
1.
Match the function in Column A with the correct blood vessel in Column B.
2.
The blood vessels that have the most elasticity are the _____________________.
3.
The blood vessels that transport blood from the lungs to the heart are the _____________________.
4.
The systemic circulatory system circulates blood through all of the body tissues except the lungs.
a) True
b) False
5.
An increase in the diameter of a blood vessel is called _________________________.
6.
Define blood pressure.
_____________________
_____________________
_____________________
7.
Match the definition in Column A with the correct term in Column B.
8.
An increase in heart rate results in increased cardiac output.
a) True
b) False
9.
Vasodilation of arteries increases peripheral vascular resistance.
a) True
b) False
10.
Stretch receptors that convey messages to the medulla about the pressure being exerted on the walls of blood vessels are called ______________________.
11.
Both alpha-1 and beta-2 receptors are found on vascular smooth muscle cells.
Alpha-1 receptors are stimulated by ______________________ and cause _____________________.
Beta-2 receptors are stimulated by ______________________ and cause ______________________.
Progress Check Answers — Section 2: Anatomy and Physiology of Blood Vessels
1.
1) c. capillaries
2) b. veins
3) a. arteries
2.
arteries
3.
pulmonary veins
4.
a) true
5.
vasodilation
6.
Blood pressure is the force exerted by the blood against the walls of the vessels.
7.
1) d. heart rate
2) a. cardiac output
3) c. stroke volume
4) b. peripheral vascular resistance
8.
a) true
9.
b) false
An increase in blood vessel size results in lowered resistance to blood flow.
10.
baroreceptors
11.
norepinephrine
vasoconstriction
epinephrine
vasodilation
Section 3: Anatomy and Physiology of the Heart
Learning Objectives
After reading this section, you should be able to:
- Describe the structure of the heart.
- Describe the pathway of blood through the heart.
- Explain the role of the coronary arteries.
- Explain the role of cardiac muscle.
- Describe the pathway of an electrical impulse through the heart muscle.
- Explain the factors involved in the generation of an action potential.
- Describe the four stages of the cardiac cycle.
- Differentiate between systolic, diastolic, and pulse pressure.
- Explain the effect of preload and afterload on stroke volume.
- State the Frank-Starling Law.
- Describe the effect of the sympathetic and parasympathetic nervous system, body temperature, and sodium, potassium, and calcium on the heart rate.
Structure of the Heart
The heart is a hollow, muscular organ that pumps blood into the blood vessels. It lies between the lungs in a compartment called the mediastinal space. The heart is shaped like a blunt cone and is about the size of a clenched fist.
The anatomical structures of the heart are divided into six groups:
-
-
- membrane (pericardium*)
- heart wall (myocardium*)
- heart chambers
- heart valves
- coronary arteries
- electrical conduction system
-
Figure 1.3-1 shows a cross section of the heart and some major blood vessels.
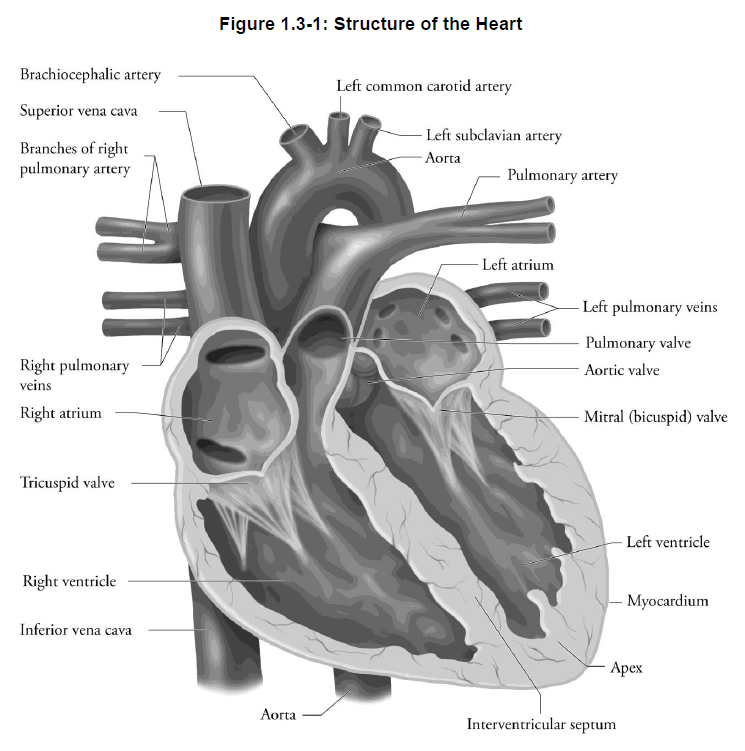
Pericardium
The pericardium (also known as the pericardial sac) is a membrane that encloses the heart and holds it in place. This structure is designed to hold the heart in place, yet allow it to move as it contracts.
The space within the pericardial sac and surrounding the heart is filled with pericardial fluid, which prevents friction between the membranes as the heart contracts.
Myocardium
The wall of the heart is divided into three sections:
-
-
- epicardium – outermost section just under the pericardium
- myocardium – thickest layer; composed of cardiac muscle
- endocardium – thin layer of cells lining the interior of the heart
-
The myocardium can be further divided into the subendocardium and subepicardium. These divisions relate to the proximity of each portion of the myocardium to the endocardium and epicardium.
Heart Chambers
The heart is divided in half with two hollow chambers or cavities on each side – the atria and ventricles. Each chamber serves as a pump to help move the blood.
1) Atria
The right and left atria (singular atrium) are the two upper chambers of the heart. They are separated by the interatrial septum*. The atria are sometimes referred to as auricles.
The atria have a relatively thin muscle wall since they only have to pump blood into the ventricles.
2) Ventricles
The two lower chambers, the right and left ventricles, are separated by the interventricular septum.
The ventricles have thicker muscle walls than the atria. The left ventricle has the thickest wall, since it delivers blood to all parts of the body, except the lungs. The right ventricle pumps blood to the lungs.
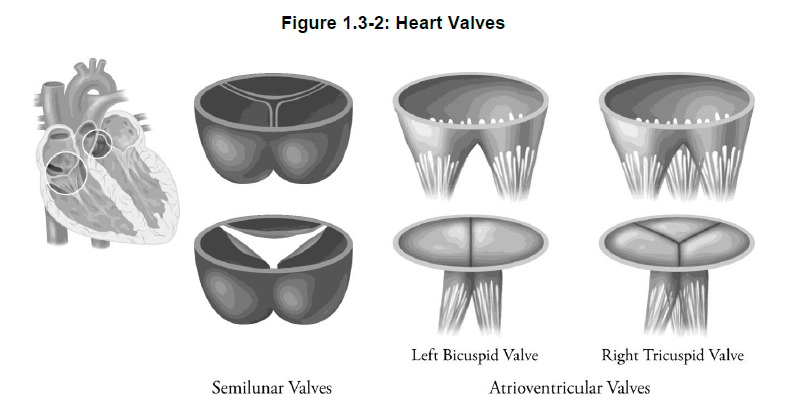
Heart Valves
Four heart valves enable the heart chambers to work as co-ordinated independent pumps. Each valve permits the blood to flow only in one direction, thus preventing the backflow of blood and ensuring blood continues to flow forward.
1) Atrioventricular (AV) valves
Atrioventricular (AV) valves are located between the atria and their respective ventricles. When the ventricles contract, these valves prevent blood from flowing from the ventricles back into the atria.
Fine tendinous cords, the chordae tendineae, are attached to the valves. These chords keep the valves from being forced into the atrium, thereby preventing backflow of blood.
The AV valve between the right atrium and right ventricle is called the tricuspid valve (or right AV valve) because it is made up of three leaflets.
The AV valve between the left atrium and the left ventricle is called the bicuspid valve or mitral valve. The mitral valve has two leaflets.
2) Semilunar valves
Two valves are located in the two major arteries that exit from the ventricles of the heart. These valves are termed semilunar valves due to their crescent or half-moon shape. They are made up of three semilunar cusps. The semilunar valves prevent blood from flowing back into the ventricles. Blood flows freely through the valves during heart contraction when the cusps are pressed against the sides of the artery. When the heart muscle relaxes, blood fills the cusps and closes the exit from the ventricles.
The pulmonary semilunar valve lies in the opening between the pulmonary artery and the right ventricle.
The aortic semilunar valve lies in the opening where the aorta exits the left ventricle.
Did You Know?
If you listen to your heartbeat, you’ll hear two sounds: lub-DUB, lub-DUB, lub-DUB. These sounds are made by the heart valves as they open and close.
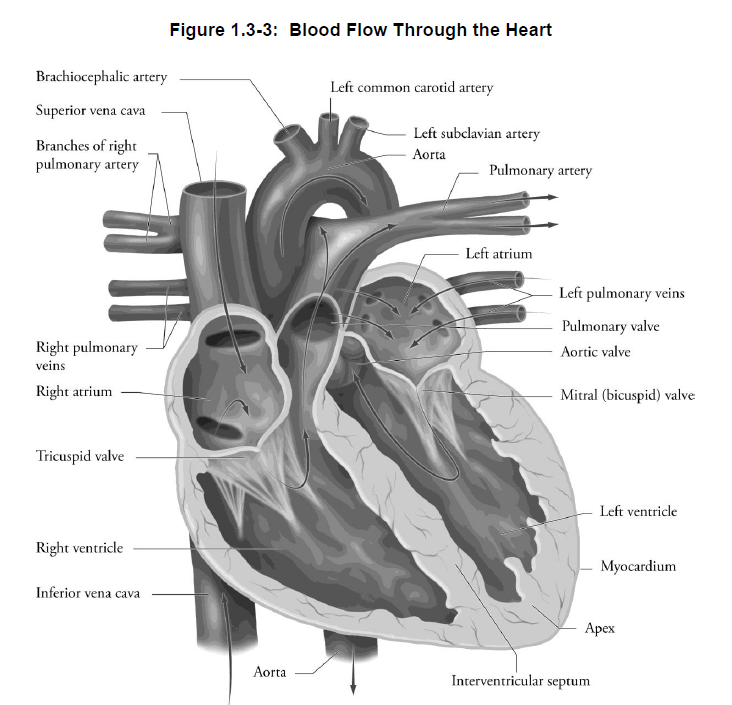
Blood Flow Through the Heart
1) Body to right atrium
The right atrium receives blood from all parts of the body except the lungs. It receives blood through three veins.
-
-
- superior vena cava – brings blood from the upper portion of the body
- inferior vena cava – brings blood from the lower portions of the body
- coronary sinus – delivers blood coming from the vessels supplying the heart muscle itself (the coronary circulation) to the right atrium
-
Blood exits the right atrium through the tricuspid valve and flows into the right ventricle.
2) Right ventricle to lungs
Blood is then pumped out of the right ventricle into the pulmonary trunk. This divides into the right and left pulmonary arteries, delivering blood to the lungs. When passing through the lungs, blood releases carbon dioxide and absorbs oxygen.
3) Lungs to left atrium
Oxygen rich blood returns from the lungs to the heart via four pulmonary veins, which empty into the left atrium. The blood flows from the left atrium through the mitral valve into the left ventricle.
4) Left ventricle to body
From the left ventricle, blood is pumped out of the heart into the ascending aorta. Blood can now be delivered to all the organs and tissues of the body, except the lungs.
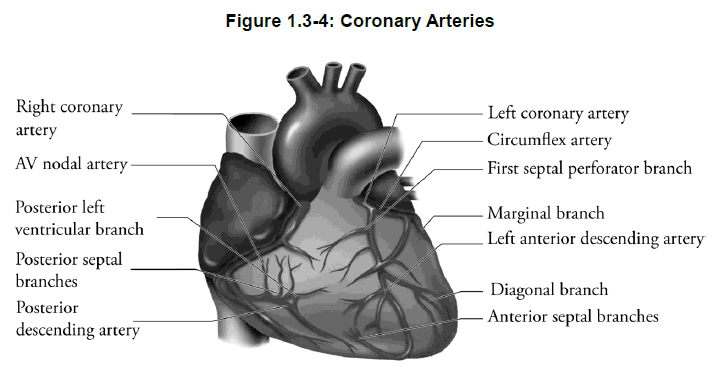
Coronary Arteries
Cardiac tissue has its own system of blood vessels that deliver nutrients and oxygen and removes wastes and carbon dioxide. The cardiac blood supply originates from the aorta via two arteries — the left coronary artery and the right coronary artery (Figure 1.3-4).
Due to the position of the coronary arteries, the heart is the first organ to receive oxygenated blood. In general, the left coronary artery delivers blood to the left side of the heart and the anterior portion of the septum while the right coronary artery delivers blood to the right side and the posterior portion of the septum.
Both arteries divide into numerous branches, which are interconnected. These interconnections provide a safety factor should an artery become occluded. The branching system of the cardiac blood supply allows every cardiac cell to be very close to a capillary.
The drainage of blood from the coronary blood vessels is primarily collected into a large venous channel, the coronary sinus, which empties into the right atrium. In addition, the anterior cardiac veins empty independently into the right atrium.
Did You Know?
Occlusion of coronary arteries is a common cause of morbidity or sudden death due to insufficient delivery of oxygen to areas of the myocardium. Interference with the blood supply results in myocardial ischemia.
Cardiac Muscle
The heart is composed of two kinds of muscle fibres: the myocardium and the specialized conduction system.
The myocardium contracts to pump blood. The walls of the atria and ventricles are composed of layers of cardiac muscle, which contract with the appropriate stimulation. Muscle fibres that contract contribute to the cardiac cycle*.
The cardiac conduction system forms branching networks that allow electrical impulses to spread easily to adjacent fibres allowing the cardiac fibres to contract as a unit.
Conduction – System Components
The specialized cardiac muscle fibres that conduct electrical impulses constitute a network known as the conduction system* of the heart (Figure 1.3-5). Most cells in this system depolarize spontaneously, which enable these cells to function as cardiac pacemakers*. The function of these specialized tissues is to generate and propagate the electrical impulse which, in turn, will initiate and co-ordinate the contraction of cardiac muscle.
There are four principal structures of the conduction system:
-
-
- sinoatrial (SA) node*
- atrioventricular (AV) node*
- bundle of His*
- Purkinje fibres*
-
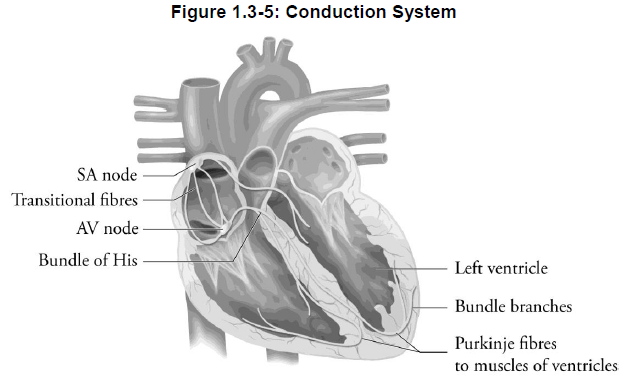
1) Sinoatrial node
The sinoatrial node (also known as the SA node) is an area of specialized tissue located in the posterior wall of the right atrium near the opening of the superior vena cava. Because electrical impulses are normally initiated in the SA node, the SA node is sometimes referred to as the heart’s pacemaker. It is the dominant pacemaker.
2) Atrioventricular node
The atrioventricular node (also known as the AV node) is an area of specialized tissue located at the base of the right atrium very near the wall between the ventricles (the interventricular septum). The AV node receives electrical impulses that reach it from the right atrium, and transmits these impulses through electrical tissue to the ventricles. The impulse is slowed.
3) Bundle of His
The bundle of His is a collection of fibres that connects the AV node and the interventricular septum. The bundle of His receives electrical impulses from the AV node and transmits them towards the ventricles.
4) Purkinje fibres
The bundle of His splits into the left bundle branch and right bundle branch, which lie on the left and right side of the interventricular septum respectively. The left and right bundle branches continue to split into Purkinje fibres, which spread the specialized conduction fibres throughout the left and right ventricles.
Did You Know?
Any alteration in the normal generation or conduction of an electrical impulse in the cardiac tissue is referred to as arrhythmia. The effect of arrhythmia on cardiac function may vary from minor palpitations to cardiac arrest, depending on the type of arrhythmia.
Conduction System – Action Potential
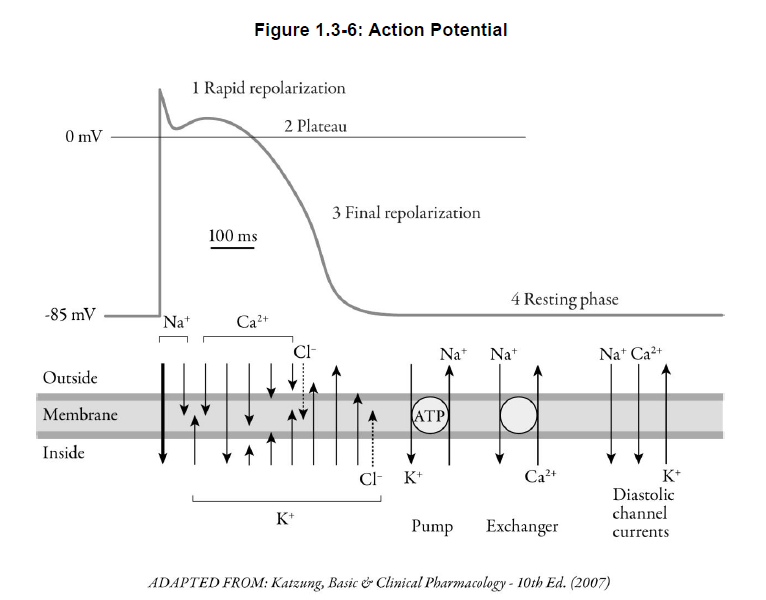
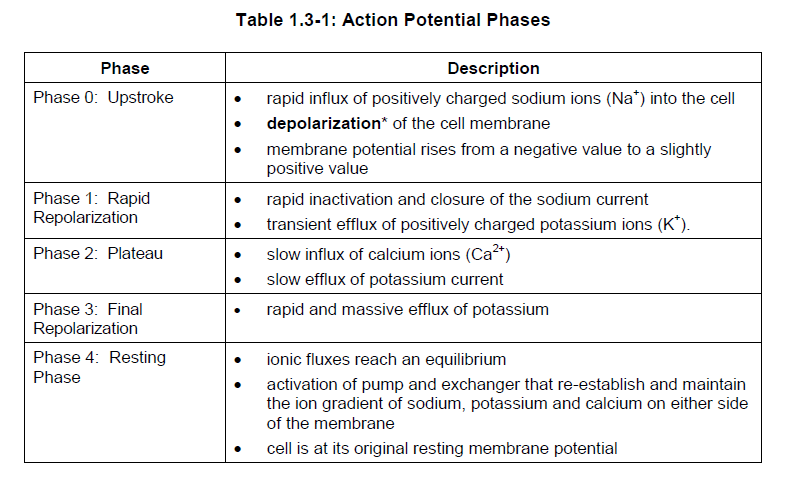
Electrical activity in the heart is generated by action potential*. The resting membrane potential of cardiac cells is -70 to -90 mv. This means that the interior of the cell is electrically negative relative to the exterior. Figure 1.3-6 shows the ion permeability changes and transport processes that occur during an action potential and the diastolic period following it. Inward (depolarizing) membrane currents are represented by arrows pointing down. Upward pointing arrows indicate outward (repolarizing) membrane currents. Chloride currents produce both inward and outward membrane currents during the cardiac action potential. Five phases are associated with the action potential of the cell.
Conduction System – Absolute Refractory Period
Cardiac cells have an absolute refractory period*. During this period, a second action potential cannot re-excite the area of cardiac tissue. The duration depends upon the rate of repolarization of the cell membrane. During the relative refractory period, the tissue can be excited by a stronger than normal stimulus.
Conduction System – Automaticity
The electrical conduction system of the heart stimulates co-ordinated propagation of the electrical impulse throughout the heart that determines rhythmic contractions of the atria and ventricles. Specialized tissue in the heart is capable of slow spontaneous generation of electrical potentials, also referred to as automaticity*. Cells capable of spontaneous depolarization are referred to as pacemaker cells.
The SA node spontaneously depolarizes at a rate of 60 to 100 times per minute. The bundle of His has a slower rate of 40 to 60 depolarizations per minute. Purkinje fibres depolarize spontaneously at a rate of 25 to 40 times per minute. Since the SA node has the highest inherent rate, it overrides the activity of all other pacemaker cells, and controls the rate of contraction of the entire heart.
Conduction System – Electrical Impulse
After the impulse originates in the SA node, it spreads through the atrial tissue, leading to contraction of the atrium. (See Figure 1.3-5.)
Next, it reaches the AV node, which controls the conduction of impulses to the ventricle. Conduction is slowed in the AV node thus allowing time for the atria to empty their contents into the ventricle.
From the AV nodal tissue, the impulse continues to travel down the common bundle of His, then through both the right and left bundle branches reaching the Purkinje fibres and finally the ventricular muscle fibres.
As the impulse passes into the ventricular conduction system, it spreads almost immediately to the entire inner surface of the ventricular muscle. This allows the ventricles to contract as a unit in response to electrical stimulation.
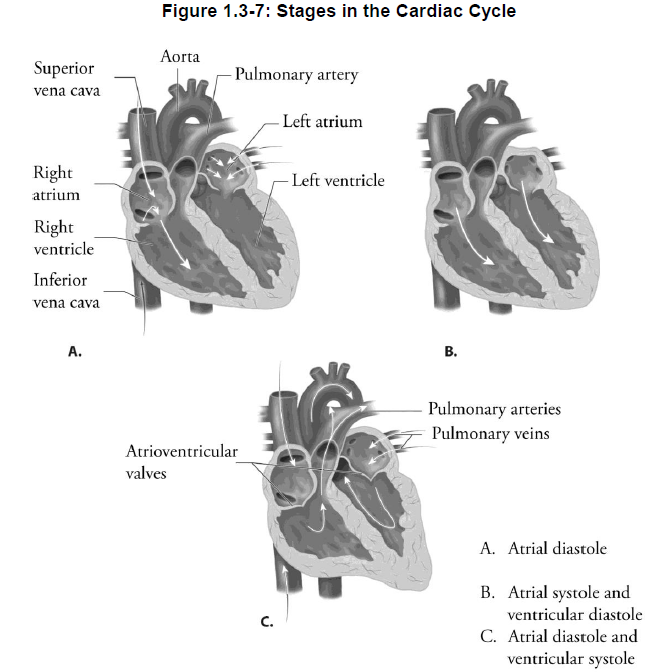
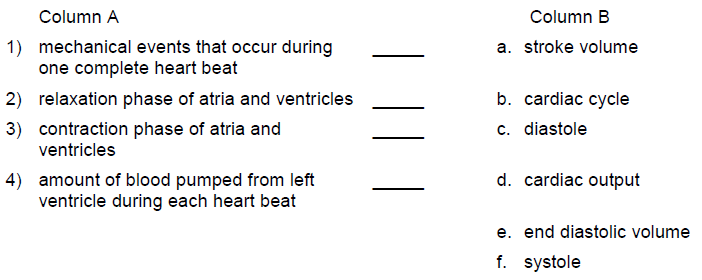
Cardical Cycle – Four Stages
The mechanical events occurring during one complete heartbeat is referred to as the cardiac cycle. The cardiac cycle consists of four stages:
-
-
- atrial diastole* – a relaxation phase of both atria
- atrial systole* – a contraction phase of both atria
- ventricular diastole – a relaxation phase of both ventricles
- ventricular systole – a contraction phase of both ventricles
-
Blood within the heart flows from an area of higher pressure to an area of lower pressure (Figure 1.3-7).
1) Atrial diastole
Beginning in atrial diastole, the right atrium receives deoxygenated blood from the superior and inferior vena cava and coronary sinus while the left atrium receives oxygenated blood from the pulmonary veins.
2) Atrial systole
As the atria are filling with blood, the pressure within the atria steadily rises. Atrial excitation then stimulates the atria to contract. The force of contraction opens the AV valves and blood is ejected into the ventricles, where the pressure is lower. During this time, the semilunar valves are closed.
Did You Know?
The heart beats about 100,000 times each day and about 35 million times in a year. During an average lifetime, it will beat more than 2.5 billion times.
3) Ventricular diastole
When the atria contract, blood is forced into the ventricles. As the ventricular muscle fibres are stretched during diastole, (filling stage) the pressure in the ventricles increases. Most of the blood flow in the coronary blood vessels takes place during ventricular diastole.
4) Ventricular systole
The ventricles are then stimulated and as they begin to contract, the pressure increases further. The pressure rises as the ventricles continue to contract until this pressure is greater than the pressure in the pulmonary and aortic vessels. The semilunar valves are forced open and blood is ejected from the ventricles. The AV valves are closed during ventricular systole.
The right ventricle pumps deoxygenated blood into the pulmonary trunk. The left ventricle forces oxygenated blood into the aorta.
Pressure falls within the ventricles as blood is ejected and the pressure from the arterial system pushes the semilunar valves closed to prevent back flow of blood into the ventricles. Both the atria and the ventricles relax (diastole) and the cycle starts over again.
Cardiac Cycle and Blood Pressure
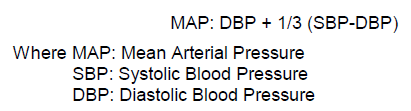
As we discussed previously, blood pressure is the force exerted by the blood against the walls of the vessels. It is measured in millimetres of mercury (mmHg).
Blood pressure varies with the amount of blood being pumped by the heart (cardiac output) and the resistance presented by the blood vessel (total peripheral vascular resistance).
The peak blood pressure value during systole is termed the systolic blood pressure (SBP)*. Normal systolic blood pressures range from 100 to 140 mmHg.
Blood pressures fall to a minimum value during diastole. This diastolic blood pressure (DBP)* is normally 60 to 90 mmHg.
Blood pressure is usually described as the systolic over the diastolic pressure. A person’s blood pressure can fluctuate considerably throughout the day and from day to day. The standard way to describe blood pressure is 120/80, where systolic pressure is 120 mmHg and diastolic pressure is 80 mmHg.
The difference between the systolic and the diastolic pressure is referred to as the pulse pressure.
The mean arterial pressure is defined as the average pressure during the cardiac cycle. An approximate estimation of mean pressure is the diastolic pressure plus one-third of the pulse pressure. A normal mean arterial pressure is about 100 mmHg.
Stroke Volume
Stroke volume (SV) is the amount of blood pumped from the left ventricle during each heartbeat. In a normal adult, stroke volume at rest is about 70 mL.
Cardiac Output
As we discussed previously, cardiac output is a measure of the volume of blood ejected from the left ventricle per minute. An average cardiac output is normally 5.25 litres per minute.
Cardiac output, also known as the cardiac index, is determined by multiplying the stroke volume (SV) by the heart rate (HR), the number of beats per minute.
![]()
The cardiac output varies depending on the demands of the body. To meet these demands, the heart adjusts the stroke volume, heart rate, or both. See Figure 1.3-8.
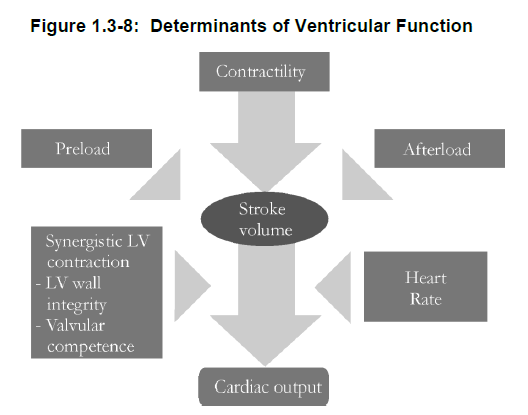
Cardiac Output – Determination of Stroke Volume
Stroke volume depends upon the mechanical properties of the heart, namely muscle length, load, and contractility.
1) Frank-Starling law or Starling’s law
In heart muscle, the initial length of the muscle fibre determines the force of contraction of the muscle fibres. This property is referred to as the Frank-Starling law* of the heart, which relates filling of the heart to the strength of contraction.
In other words, when diastolic filling increases there is an increase in muscle fibre stretch, which results in an increased force of heart muscle contraction.
An increased volume of blood in the ventricle stretches the myocardial muscle. This results in increased myocardial contraction and ejection of the excess blood volume. An increase in SV and CO is observed. However, if excessive muscle stretch occurs, myocardial contractions weaken and heart failure ensues.
2) Preload
The amount of blood the ventricles receive during diastole is referred to as the end diastolic volume (EDV)*. The EDV is determined by the length of diastole and the venous pressure.
The final pressure generated by the EDV is also referred to as preload*. If there is a small volume of blood in the ventricles, preload is low.
End systolic volume (ESV)* is the volume of blood that is left in the ventricle after systole. This volume is determined by the force of contraction and the arterial pressure.
3) Afterload
The load against which the heart has to pump, or afterload*, also affects stroke volume. This is determined by pressure in the arteries, also referred to as peripheral vascular resistance. Peripheral vascular resistance is the impediment to blood flow in peripheral blood vessels. Vasoconstriction increases peripheral vascular resistance, thereby increasing afterload. Increased afterload results in increased work for the heart and a reduced stroke volume.
Did You Know?
EDV is the amount of blood in the ventricle immediately before a cardiac contraction begins. It is a measurement of cardiac filling between beats, i.e., diastolic function. ESV is the amount of blood in the ventricle at the end of the cardiac ejection period and immediately preceding the beginning of ventricular relaxation. It is a measurement of the adequacy of cardiac emptying, i.e., systolic function.
Cardiac Output – Determination of Heart Rate
The heart rate varies depending upon stimulation of the autonomic nervous system (ANS) and numerous chemical factors.
1) ANS
Sympathetic nerves increase the heart rate. Parasympathetic nerves decrease the heart rate.
2) Body temperature
Body temperature may influence cardiac conduction. Increased temperature will stimulate the SA node to increase heart rate.
3) Sodium, potassium and calcium
Significant variations in body concentrations of sodium, potassium and calcium will also affect cardiac electrical activity.
Large decreases in serum sodium (hyponatremia*) and potassium (hypokalemia*) will affect cardiac action potential configuration and resting membrane potential. This may lead to arrhythmias*.
Increases in potassium (hyperkalemia*) may lead to arrhythmias due to the greater ease of depolarization.
Increased serum calcium (hypercalcemia*) will increase the force of contraction, because more calcium is available to the muscle fibres.
Summary — Section 3: Anatomy and Physiology of the Heart
The heart is a four-chamber pump made up of two atria and two ventricles. The atria move blood into the ventricles. Contraction of the ventricles provides the force to deliver blood through the lungs and the rest of the body. Four heart valves permit blood flow in only one direction through the heart. This ensures that the chambers work as co-ordinated independent pumps. Coronary arteries that originate from the aorta supply blood to cardiac tissue.
The electrical conduction system of the heart generates and propagates the electrical impulse which, in turn, will initiate and co-ordinate the contraction of the atria and ventricles. Electrical activity in the heart is generated by action potential. The action potential is generated in five phases. The SA node pacemaker normally controls the rate of the electrical activity of the heart. Conduction originates in the SA node, spreads through the atria and AV node, continues down the common bundle of His, and eventually reaches the Purkinje fibres, which propagate into the ventricular muscle.
The cardiac cycle describes the process whereby the co-ordination of atrial and ventricular contraction and relaxation results in ejection of blood from the heart. The heart maintains an adequate cardiac output by varying either heart rate and/or factors, which affect stroke volume. According to the Frank-Starling law, the myocardium can vary its CO based on the amount of diastolic filling or stretch of the myocardial wall. Cardiac workload can be described in terms of preload and afterload. These “loads” refer to the input of blood to the heart and resistance to ejection of blood from the heart respectively. An increase in load to the heart will increase the work it will perform.
Physiologic control of the heart rate is influenced by the autonomic nervous system, body temperature and serum concentrations of sodium, potassium, and calcium.
Progress Check — Section 3: Anatomy and Physiology of the Heart
1.
The membrane surrounding the heart is called the ____________________________.
2.
Another name for cardiac muscle is ______________________________.
3.
List in the correct order each part of the heart and the major blood vessels a blood cell would pass through from the time it arrives at the heart in the inferior vena cava until it leaves the heart in the aorta.
1) inferior vena cava
2) ________________________________
3) ________________________________
4) ________________________________
5) ________________________________
6) ________________________________
7) ________________________________
8) ________________________________
9) ________________________________
10) _______________________________
11) _______________________________
12) _______________________________
13) aorta
4.
Describe the pathway of an electrical impulse through the heart muscle.
____________________________
____________________________
____________________________
____________________________
5.
While visiting his physician for his annual check-up, MV was told his blood pressure is 130/82.
1) What is MW’s diastolic blood pressure?
____________________________
2) What is MW’s systolic blood pressure?
____________________________
3) Is MW’s systolic blood pressure within the normal range? Explain.
____________________________
____________________________
6.
Match the description in Column A with the correct term in Column B.
7.
Explain how preload affects stroke volume.
_____________________________
_____________________________
_____________________________
_____________________________
8.
Explain how afterload affects stroke volume.
_____________________________
_____________________________
_____________________________
_____________________________
9.
State the Frank-Starling law.
_____________________________
_____________________________
_____________________________
_____________________________
10.
Heart rate increases in response to stimulation of ______________________ nerves.
11.
What effect might an increase in calcium have on the heart?
_____________________________
_____________________________
_____________________________
_____________________________
12.
If a person develops weakness or damage to the mitral valve, what would the consequences be?
_____________________________
_____________________________
_____________________________
_____________________________
Progress Check Answers — Section 3: Anatomy and Physiology of the Heart
1.
pericardium
2.
myocardium
3.
1) inferior vena cava
2) right atrium
3) tricuspid valve
4) right ventricle
5) semilunar valve (pulmonary valve)
6) pulmonary artery
7) lungs
8) pulmonary veins
9) left atrium
10) mitral (bicuspid) valve
11) left ventricle
12) semilunar valve (aortic valve)
13) aorta
4.
An electrical impulse originates in the SA node, spreads through the atria and AV node, continues down the common bundle of His, and eventually reaches the Purkinje fibres, which propagate into the ventricular muscle.
5.
1) 82 mmHg
2) 130 mmHg
3) Yes. The normal range for systolic blood pressure is 100-140 mmHg.
6.
1) b. cardiac cycle
2) c. diastole
3) f. systole
4) a. stroke volume
7.
Preload is the pressure caused by the volume of blood received by the ventricles during diastole. If there is a small volume of blood in the left ventricle, preload is low resulting in a lowered stroke volume. The higher the preload, the greater the pressure on the myocardium, resulting in increased myocardial contractility and increased stroke volume. This principle follows the Frank-Starling Law.
8.
Afterload is the load or resistance against which the heart has to pump. Increased afterload results in increased work for the heart and a reduced stroke volume.
9.
In heart muscle, the initial length of the muscle fibre determines the force of contraction of the muscle fibres. An increased volume of blood in the ventricle stretches the myocardial muscle, resulting in increased myocardial contraction and ejection of a greater volume of blood volume.
10.
sympathetic
11.
Increased calcium concentration increases the force of contraction of the heart.
12.
Damage to the mitral valve will allow back flow of blood from the left ventricle into the left atrium. This will result in a reduced stroke volume from the left ventricle during systole.
Section 4: Function and Composition of Blood
Learning Objectives
After reading this section, you should be able to:
- State the three main functions of blood.
- State the function of plasma, erythrocytes, leukocytes and platelets.
- Explain the role of the prostaglandins thromboxane A2 and prostacyclin in the formation of a platelet plug.
- Explain the role of thrombin and fibrin in the formation of a blood clot.
- Explain the role of the fibrinolytic system in the blood clotting process.
Functions of Blood
Circulating blood serves the body in three ways:
-
-
- transportation – carries oxygen, nutrients, hormones, electrolytes and heat to every living cell, and collects wastes such as carbon dioxide, urea, extra water and heat from the cells
- regulation – aids in the regulation of body temperature, the amount of fluid in the tissues, acid-base balance of the body fluids, and coagulation of blood
- protection – carries cells that help protect the body against disease-causing microorganisms. It also contains antibodies that play a role in immunity against disease.
-
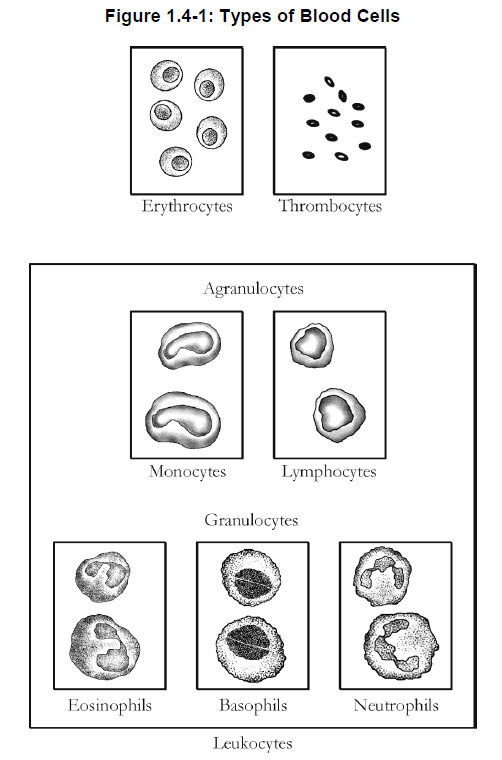
Composition of Blood
Blood is composed of a liquid portion called plasma* and cells.
The cells include:
-
-
- erythrocytes (red blood cells)
- leukocytes (white blood cells)
- platelets* (thrombocytes)
-
See Figure 1.4-1
1) Plasma
Over half of the total volume of blood is plasma.
Plasma is 90% water. Other components of plasma include:
-
-
- proteins such as albumin, antibodies, and clotting factors
- nutrients such as glucose, amino acids, and lipids
- electrolytes such as sodium, potassium, chloride and calcium
- hormones
- waste products such as urea and lactic acid
- respiratory gases such as oxygen or carbon dioxide
-
2) Erythrocytes
Erythrocytes are the red blood cells. They transport oxygen from the lungs to the tissues. In the erythrocytes, the oxygen is bound to hemoglobin*, which is an iron-containing protein. When hemoglobin combines with oxygen, the blood has a red colour.
Production of erythrocytes is stimulated by the hormone erythropoietin*, which is produced in the kidney in response to a low oxygen level in the blood.
3) Leukocytes
Leukocytes, or white blood cells, are involved in the body’s immune response and protect the body against infections by destroying invading pathogens*.
There are several types of leukocytes. When pathogens enter the tissues, specific white blood cells are attracted to the site of infection. They move from the blood vessels to the area of infection and engulf the pathogens by the process of phagocytosis*.
4) Platelets
Platelets (thrombocytes) are the smallest of the formed elements and are fragments of cells. Platelets are essential to the blood clotting process.
Did You Know?
The average life span of an erythrocyte is approximately 120 days. This means that almost 1% of the body’s erythrocytes must be replaced every day.Anemia is a disorder in which there is an abnormally low level of hemoglobin or erythrocytes in the blood. Leukemia is a malignant disease characterized by proliferation of abnormal leukocytes in blood and bone marrow.
Blood Clotting
1) Platelet plug
Platelets are not normally attracted to the endothelium of a blood vessel. When injury occurs to the vascular endothelium, the platelets become activated and begin to adhere to collagen on the exposed vessel wall.
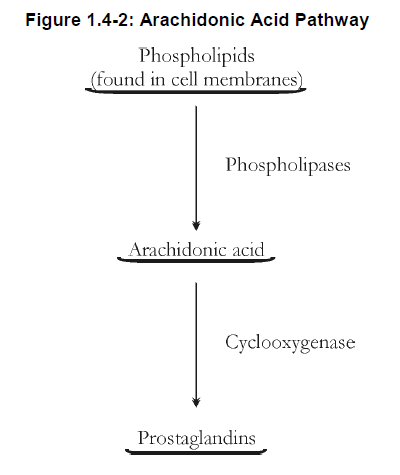
Due to activation of the arachidonic acid pathway, the activated platelets begin to secrete several compounds that cause circulating platelets to stick together (aggregate) and form a platelet plug.
Transformation of this temporary platelet plug to a permanent platelet-fibrin clot is achieved through the subsequent activation of the coagulation system (blood clotting system).
2) Role of prostaglandins
Arachidonic acid, from membrane-bound phospholipids, is the precursor of several prostaglandins* that affect platelet function. The enzyme cyclooxygenase* plays an important role in the metabolic pathways that lead to the production of these prostaglandins. See Figure 1.4-2.
The prostaglandin thromboxane A2* stimulates platelet aggregation and causes vasoconstriction.
Prostacyclin*, another prostaglandin, inhibits platelet aggregation and causes vasodilation. Prostacyclin limits the size of the platelet plug.
Did You Know?
ASA (acetylsalicylic acid) works by irreversibly inhibiting cyclooxygenase-1 enzyme (COX-1) in platelets. This prevents the formation of further thromboxane A2, and therefore reduces platelet aggregation.
3) Clotting factors
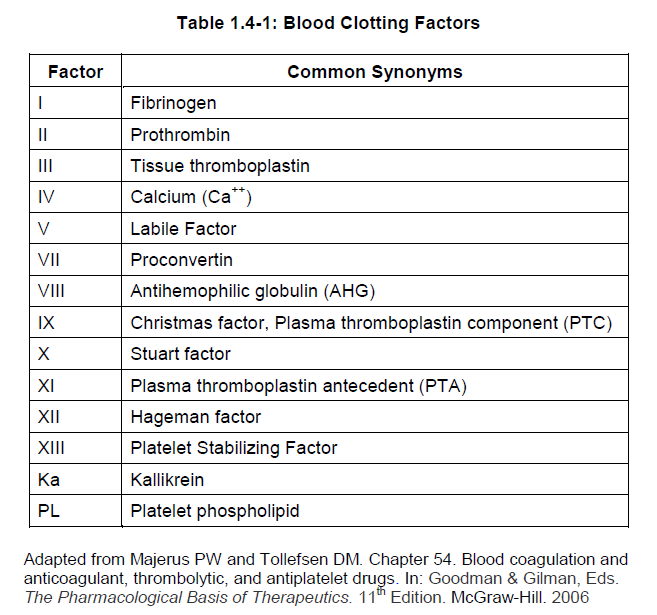
Clotting factors (also known as coagulation factors) are circulating plasma proteins. Clotting factors are inactive forms of enzymes normally present in the blood. They are activated when vascular endothelium is injured. Table 1.4-1 lists the clotting factors. Notice that most of them are assigned a Roman numeral.
4) Clotting process
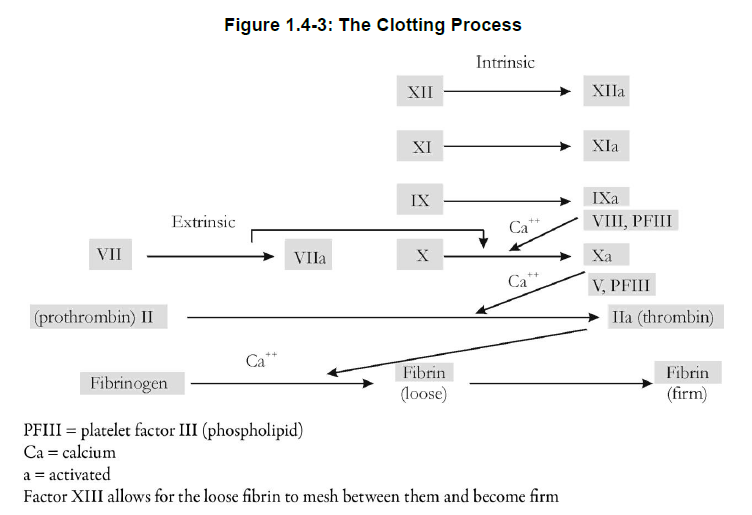
The formation of a thrombus* is the result of a complex series of steps leading to the production of fibrin* (see Figure 1.4-3). A proenzyme is converted to an enzyme. The new enzyme then activates the next proenzyme in the series.
Injury to vascular endothelium stimulates platelets and initiates a cascade of reactions within the intrinsic pathway of the coagulation system. The coagulation factors are activated, with the eventual formation of fibrin.
An alternate pathway to the formation of fibrin is via the extrinsic pathway. These two pathways amplify the production of thrombin* (factor IIa), the common link between the two pathways.
Did You Know?
Hemophilia is a genetic disorder characterized by a deficiency of certain clotting factors. Any cut or bruise may cause serious abnormal bleeding. Thrombocytopenia is caused by a deficient number of circulating platelets. It results in hemorrhages in the skin or mucous membranes.
5) Fibrinolytic system
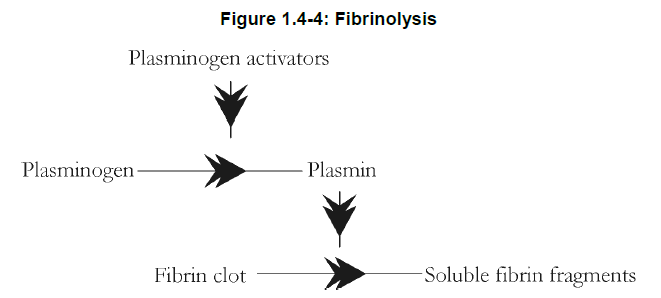
The fibrinolytic system counterbalances the complex cascade of the coagulation system, and provides protection against excessive clotting. The circulating plasma protein plasminogen* plays a key role.
Plasminogen can be activated by plasminogen activators, to an active proteolytic enzyme known as plasmin*. Plasmin lyses or breaks up the fibrin contained within a clot. See Figure 1.4-4.
There is a naturally occurring tissue-type plasminogen activator (TPA)* that is released when a thrombus is formed. This plasminogen activator is released only at the site of the thrombus.
As a result, the effect is concentrated to that area, and bleeding complications in other areas of the body are prevented.
Urinary-type plasminogen activator (urokinase*) is present in plasma at low levels, but plays a secondary role to TPA.
Did You Know?
Thrombolytic agents (e.g., alteplase) are a recombinant DNA-derived form of the naturally occurring human tissue-specific plasminogen activator.
Summary — Section 4: Function and Composition of Blood
Blood contains cells plus plasma. Erythrocytes transport oxygen to the tissues, leukocytes are involved in immune function and protect the body against infection, and platelets are essential for blood clotting.
Platelet function is affected by the prostaglandins thromboxane A2 and prostacyclin produced from arachidonic acid in the presence of the cyclooxygenase enzyme.
The clotting process involves a series of reactions in which clotting factors are activated, resulting in the formation of fibrin. Thrombin, in the presence of calcium, aids in the conversion of fibrinogen to fibrin.
The fibrinolytic system counterbalances the complex cascade of the coagulation system. It provides protection against excessive clotting. Plasmin, formed from plasminogen, lyses the fibrin contained in a clot.
Progress Check — Section 4: Function and Composition of Blood
1.
What are the three main functions of blood?
1 _____________________________
2 _____________________________
3 _____________________________
2.
The blood cells that transport oxygen are the _____________________________.
3.
Oxygen is bound to ______________________.
4.
The blood cells that protect the body against infection are the _____________________.
5.
The prostaglandin that stimulates platelet aggregation is ____________________.
6.
The clotting factor thrombin is necessary to convert ___________________________ to ______________________.
7.
Plasminogen activators convert plasminogen to ______________________________.
8.
Fibrin clots are lysed by ______________________.
9.
What is the purpose of a platelet plug?
__________________________
__________________________
Progress Check Answers — Section 4: Function and Composition of Blood
1.
1) transportation of oxygen, nutrients, hormones, electrolytes and heat to cells and wastes and extra heat away from cells
2) regulation of body temperature, tissue fluid volume, acid-base balance of body fluids, and coagulation
3) protection against disease
2.
erythrocytes (red blood cells)
3.
hemoglobin
4.
leukocytes (white blood cells)
5.
thromboxane A2
6.
fibrinogen
fibrin
7.
plasmin
8.
plasmin
9.
A platelet plug prevents blood loss after injury to a blood vessel.
Module 1 Test
1.
Which blood vessels contain the largest amount of elastic tissue?
a) capillaries
b) arterioles
c) venules
d) arteries
2.
Arrange the following blood vessels in the proper sequence of blood flow in the systemic circulation (starting at the heart):
1) veins ____________
2) arteries ____________
3) venules ____________
4) arterioles ____________
5) capillaries ____________
3.
Indicate whether each of the following statements is True or False.
1) The capillaries are the major vessels that allow the exchange of materials between blood and cells. True False
2) The pulmonary veins carry deoxygenated blood from the heart to the lungs. True False
3) Of the various blood vessels, arterioles play the greatest role in regulating blood pressure. True False
4.
Which of these vessels would you expect to have the lowest blood pressure?
a) arteries of the leg
b) coronary arteries
c) capillaries
d) veins of the leg
5.
Which of the following responses is observed with stimulation of the alpha-1 receptor?
a) increased heart rate
b) increased cardiac conduction
c) increased myocardial contractility
d) vasoconstriction of blood vessels
6.
The membrane which surrounds the heart is called the ______________________.
7.
The ______________________ valve separates the right atrium from the right ventricle?
8.
What is the function of the pulmonary veins?
_______________________________
_______________________________
9.
Which is the normal sequence of conduction of electrical impulses in cardiac tissue?
a) AV node, atria, SA node, Purkinje fibres, Bundle of His
b) SA node, Purkinje fibres, atria, AV node, Bundle of His
c) SA node, atria, AV node, Bundle of His, Purkinje fibres
d) SA node, atria, AV node, Purkinje fibres, Bundle of His
10.
The SA node is the heart’s primary pacemaker due to its:
a) relatively higher firing rate
b) relative refractory period
c) pulse pressure
d) ejection fraction
11.
Blood is pumped from the heart during:
a) atrial diastole
b) atrial systole
c) ventricular diastole
d) ventricular systole
12.
According to the Frank-Starling law of the heart:
a) increased diastolic filling results in an increased force of contraction
b) increased end-systolic volume results in an increased force of contraction
c) increased afterload results in an increased force of contraction
d) increased firing of baroreceptors stimulates the cardio-inhibitory centre
13.
Afterload can be increased by:
a) vasodilation of arterioles
b) vasoconstriction of arterioles
c) excess fluid volume
d) increased heart rate
14.
The function of erythrocytes is to:
a) transport oxygen to the tissues
b) destroy invading pathogens
c) aid in blood clotting
d) activate the arachidonic acid pathway
15.
During the formation of a thrombus, which of the following is produced?
a) urokinase
b) fibrin
c) plasminogen
d) plasmin
16.
Which of the following is a clotting factor required to convert fibrinogen to fibrin?
a) thrombin
b) thromboxane A2
c) plasmin
d) hemoglobin
17.
SR is a 53-year-old male who complains of shortness of breath, weakness, and pain in the left chest. On examination, SR’s physician determined that the valve in SR’s heart between the left ventricle and aorta is not functioning properly.
1) What is the name of the valve located between the left ventricle and aorta?
________________________
2) Assessment determined that SR’s heart valve does not close properly. Why would this be a disadvantage?
________________________
________________________
________________________
________________________
3) What physiological adjustments might partially overcome the disadvantages?
________________________
________________________
________________________
________________________
Module 1 Test Answers
1.
d) arteries
2.
1) arteries
2) arterioles
3) capillaries
4) venules
5) veins
3.
1) True
2) False Pulmonary veins transport oxygenated blood from the lungs back to the heart.
3) True
4.
d) veins of the leg
5.
d) vasoconstriction of blood vessels
6.
pericardium
7.
tricuspid valve
8.
The pulmonary veins transport oxygenated blood from the lungs to the heart.
9.
c) SA node, atria, AV node, Bundle of His, Purkinje fibres
10.
a) relatively higher firing rate
11.
d) ventricular systole
12.
a) increased diastolic filling results in an increased force of contraction
13.
b) vasoconstriction of arterioles
14.
a) transport oxygen to the tissues
15.
b) fibrin
16.
a) thrombin
17.
1) aortic valve (semilunar valve)
2) If the aortic valve does not function properly, oxygenated blood will back flow into the left ventricle instead of being pushed into the aorta for delivery to the body tissues. This will lead to increased volume in the ventricle, i.e., increased end systolic volume, decreased cardiac output, and less oxygenation of tissues in the body.
3) Initially, the heart would pump less blood from the left ventricle. This results in an increased volume of blood remaining in the ventricle (increased preload) and increased pressure within the left ventricle (left ventricular end-diastolic pressure). Normally, the heart senses the additional blood volume remaining in the ventricle due to the increase in preload, and increases the force of myocardial contraction in an attempt to eject the excess blood volume (i.e., attempts to increases stroke volume and cardiac output). This compensation through the Frank-Starling mechanism may work for a while, but the increased preload may result in myocardial dysfunction caused by excessive stretching of myocardial muscle fibres, resulting in heart failure.
